Garbow/Neil/Ackerman Lab
Projects
Is Cortical Expansion Sufficient to Drive Normal and Aberrant Brain Structure?
In human brain development, the third trimester represents a critical period of cortical expansion, folding, and white matter organization. Deviations from the normal developmental trajectory have been linked to abnormal cortical morphologies and white matter organization, which in turn have been linked to disorders including epilepsy, developmental delay, autism spectrum disorder, schizophrenia, anxiety, and depression. However, the mechanisms underlying folding, and hence the etiology of folding abnormalities, are the subject of active debate.
Cellular and Molecular Mechanisms of Postpartum Uterine Involution: Impact of Cesarean Delivery (C/S)
The uterus is a dynamic organ, crucial for the development of the offspring via implantation, placentation, and the delivery of the newborn and placenta at parturition. However, following delivery, the dramatic uterine changes that occur during pregnancy and parturition must be resolved via the process of uterine involution, which includes repair and remodeling of uterine tissue to aid in recovering its histoarchitecture and function. If postpartum uterine involution is abnormal, it may adversely affect the health of the mother by impairing her future fertility and increasing her risk of hemorrhage, miscarriage, abortion, abnormal placentation, placenta accrete spectrum (PAS), uterine rupture, or death. The detailed cellular and molecular mechanisms of postpartum uterine involution are poorly understood, and in particular after cesarean delivery (C/S).
Impact of Radiation Biology on Glioblastoma Immune Therapy
Standard of care for newly diagnosed glioblastoma (GBM) employs chemo-radiation treatment as a key therapeutic modality. Unfortunately, nearly every GBM recurs, with the great majority located within or along margins of the radiation treatment field. Recurrent GBM displays a distinctly more aggressive phenotype and increased resistance to treatment compared to newly diagnosed GBM. While immunotherapy has enjoyed considerable success in many cancers, it has been disappointing in early clinical trials in GBM. A non-invasive imaging metabolic signature that can provide insight into the aggressive phenotype and efficacy of immunotherapy would have considerable clinical value.
Distinguishing Recurrent Brain Tumor from Radiation Necrosis
Distinguishing recurrent brain tumor from treatment effects, including late time-to-onset radiation necrosis (RN), presents an important on-going diagnostic dilemma in neuro-oncology. Delayed post-radiation changes and recurrent tumor are characterized by overlapping MRI features that limit the ability of standard-of-care neuro-oncology MRI protocols to consistently distinguish RN from recurrent tumor. The heterogeneity and variability of tumors growing in-and-around irradiated surgical cavities, in the location where tumors typically recur, often confounds MRI findings. Magnetic susceptibility-induced artifacts arising from residual blood, calcified tissue, or nearby bony anatomy further compromise MRI of the post-treatment brain, especially Dynamic Susceptibility Contrast (DSC)-derived CBV signatures. As a result, imaging information is often indeterminate. Accurate clinical diagnosis is required to provide patients with appropriate treatment. Identifying tumor recurrence in a background of RN distinct from RN alone – an unsolved problem – is an important unmet clinical need.
The Ketogenic Diet (KGD) in Mouse Models of Epilepsy: A Deuterium Metabolic Imaging Study
The ketogenic diet (KGD) is widely used as an anti-seizure therapy for patients with epilepsy. Despite having been in use in some form for over a century, the mechanism(s) underlying its therapeutic effect are not as yet well understood. However, it is likely that its mechanism of action involves alterations in energy metabolism because the primary energy substrate in brain shifts from glucose to ketone bodies in patients on the KGD. In patients on a normal diet, the tricarboxylic acid (TCA) cycle is driven mainly by the formation of pyruvate via glycolysis. Under the conditions of the KGD, glucose availability is reduced, and the TCA cycle is driven mainly by ketones (acetoacetic acid and -hydroxybutyrate) entering the TCA cycle via conversion to acetyl-CoA.
Imaging and Targeted Auger Radiotherapy of High-Grade Glioma
(1 of 2)
Glioblastoma (GBM) is a highly aggressive, malignant, primary brain tumor. Maximal neurosurgical tumor resection, followed by highly conformal radiation and concurrent chemotherapy, remains the standard of care for GBM patients. These tumors inevitably recur. Given the dismal prognosis, improved technologies are desperately needed to enable better treatment of recurrent GBM. An additional complicating factor is the diagnostic challenge of non-invasively discriminating recurrent GBM from radiation necrosis (RN). PARP-1, an enzyme involved in DNA repair, is selectively overexpressed in the nuclei of glioma cells.
Imaging and Targeted Auger Radiotherapy of High-Grade Glioma
(2 of 2)
Early detection of Alzheimer’s disease (AD) remains a critical unmet clinical need. Poly(ADP-ribose) polymerase-1 (PARP-1) is a DNA repair enzyme that regulates the expression of pro-inflammatory factors. Microglia, the primary inflammatory cellsof the brain, are intimately associated with amyloid plaques in the brains of patients with AD. It has been shown that the response of microglia to neuroinflammation is mediated by PARP-1 and that PARP-1 inhibition or knockout in transgenic AD mice has a beneficial effect on cognitive dysfunction, synaptic damage, and microglial activation. To date, however, there have been no studies that have investigated a radiolabeled PARP-1 imaging agent for determining PARP-1 expression in AD mice and correlating the imaging findings with AD pathology. Building on our preceding project, which focuses on the development of radiolabeled PARP-1 inhibitors that can be used as tracers for non-invasive positron emission tomographic (PET) imaging of recurrent glioma, in this project we test the hypothesis that similar inhibitors can be used to non-invasively track neuroinflammation related to AD pathology.
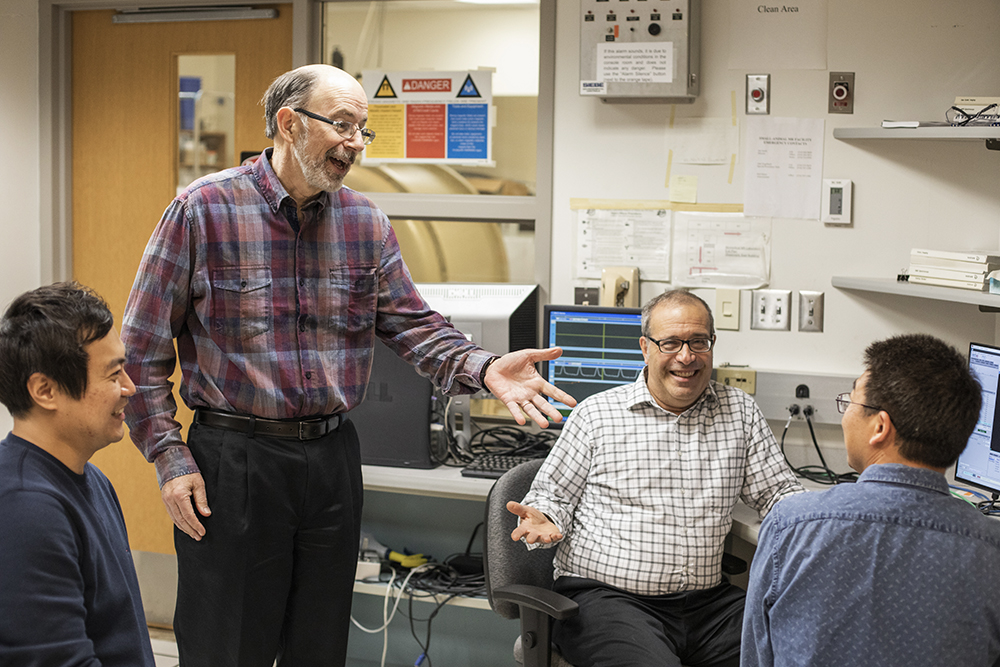
Our People
The lab partners with Washington University’s leading researchers in the field of magnetic resonance imagine (MRI) and magnetic resonance spectroscopy (MRS).