A Better Way to See Prostate Cancer
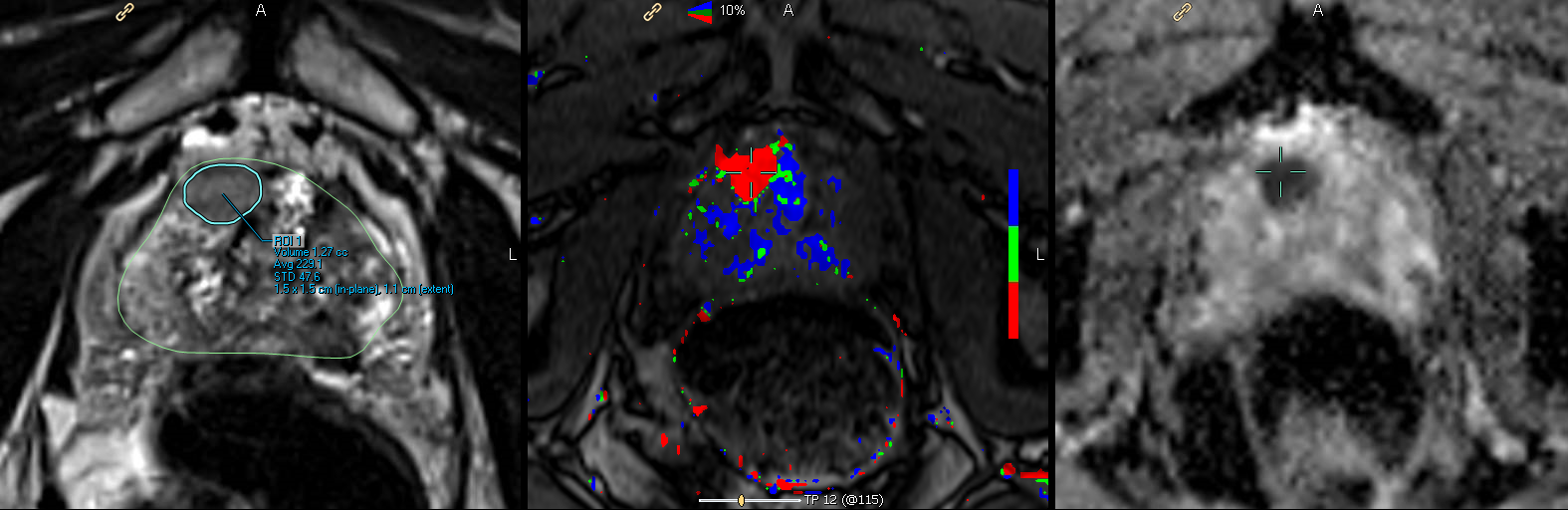
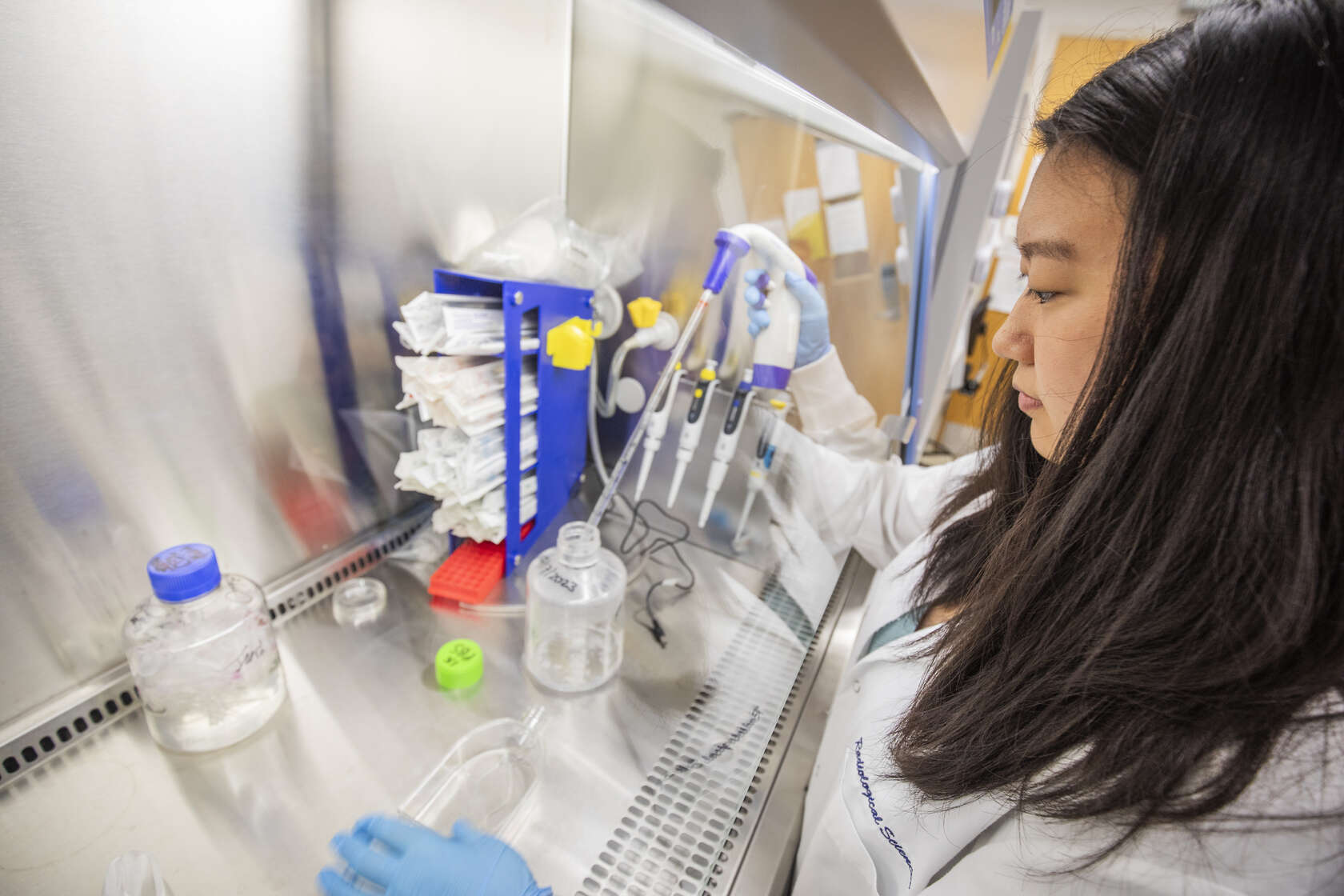
Traditionally, a prostate biopsy is performed with an ultrasound. A probe called a transducer is inserted in the rectum to obtain images of the prostate’s anatomy. If suspicious lesions are detected, a needle is advanced through the wall of the rectum into the prostate to extract tiny tissue samples. A minimum of 12 samples is needed. At best it’s a scattershot approach: not all prostate cancers are visible with ultrasound.
Prostate MRI (magnetic resonance imaging) is improving the odds of finding hidden cancer.
“MRI provides guidance for the ultrasound biopsy,” says Kathryn Fowler, MD, assistant professor of radiology. “Prostate biopsy is still technically an ultrasound-guided procedure, however, the findings from the MRI are fused with the ultrasound images to provide exact coordinates for sampling the region of interest.” Translation: It’s more accurate.
“We use prostate MRI to stage known cancers prior to surgery or radiation therapy, to diagnose and conduct pre-biopsy planning for patients with suspected cancer and to monitor those men with known ‘low-risk’ cancers,” Fowler says.
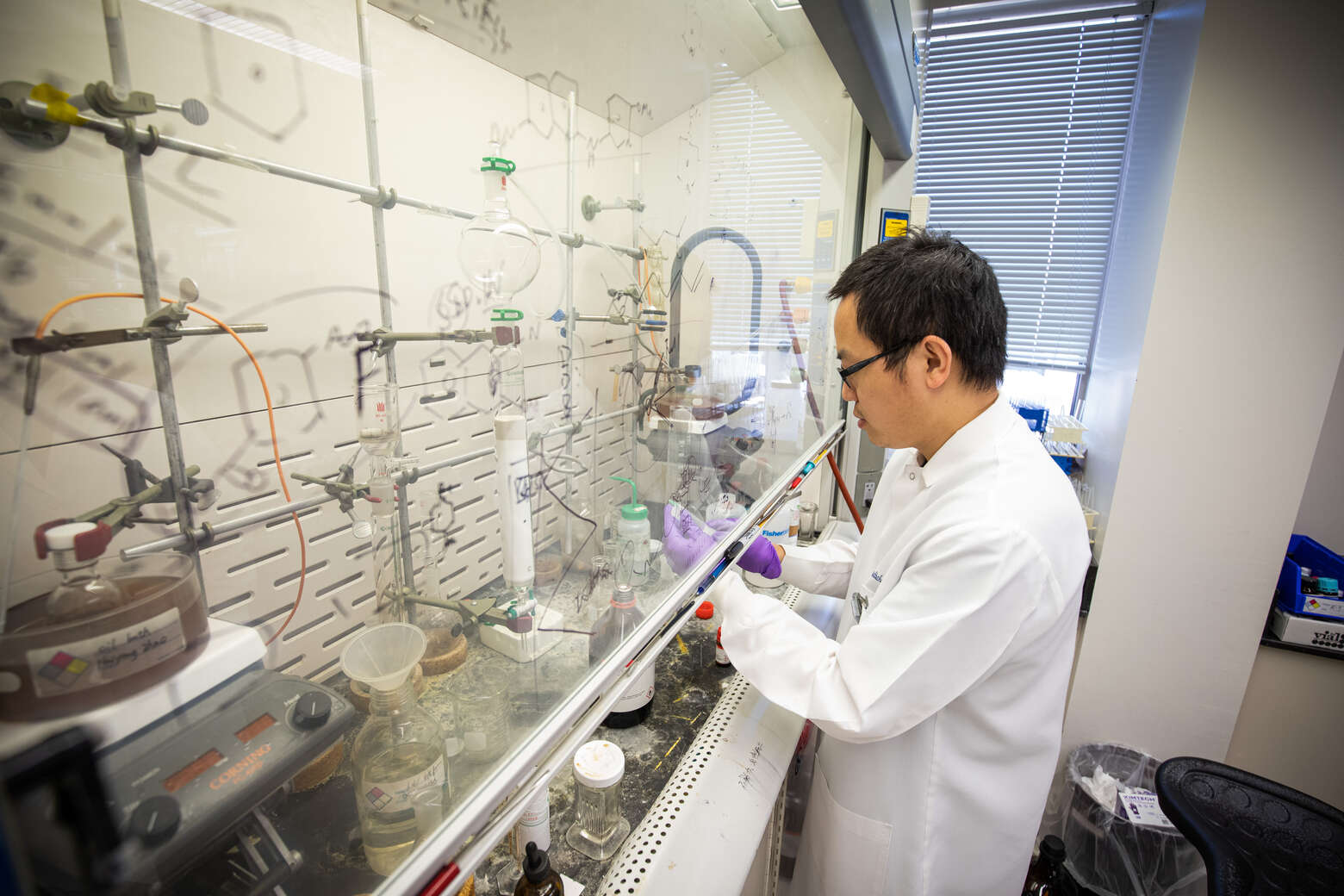
But it’s not just any MRI. “We perform all of our (prostate) imaging with a 3Tesla (3T) MRI,” continues Fowler. “3T is a higher-strength magnet that provides more signal power (tumors are more conspicuous from the background) and offers better spatial resolution (structures appear clearer).” MRI use magnet, not radiation, to produce images.
Studies have shown that 3T MRI are essential for optimal prostate imaging. “That’s because the prostate is relatively small, located deep in the pelvis and that differentiating the tumor from an enlarged prostate or inflammatory changes is challenging,” Fowler says.
And just as magnet strength matters in a prostate MRI, so does expertise of those reading the images.
“Several sites have 3T magnets, however, not everyone in the community is an expert in producing images of the prostate. Unfortunately, the images acquired at non-specialized sites are often not adequate for interpretation, even for a second opinion.”
Adds Washington University School of Medicine chief of urologic surgery Gerald Andriole, MD, “Prostate MRI has revolutionized our ability to find prostate cancer and to properly assess its size and location. Often, when we know exactly where the cancer is located in the prostate, we can offer less invasive treatments that are apt to be as effective with fewer side effects.”
September is National Prostate Cancer Awareness Month. In 2016, approximately 180,000 men will be diagnosed with the disease. Men who are African-American, over 65 years of age or who have a family history of prostate cancer are at greatest risk.